Coronary Angiography: Heart Test, Recovery & Risk
Coronary Angiography: Heart Test, Recovery & Risk
What is angiography and how is it done?
An angiogram of the heart is a special X-ray test. It is done to take pictures of the blood flow in an artery or a vein. This test is carried out using a technique called catheterization which involves the use of catheters and X-ray. An angiogram is done to find out if there is any abnormality in the blood vessels, to detect a blockage, to know the extent of a blockage, and to decide the most suitable treatment for the patient. An angiogram may be done in any blood vessel throughout the body. Special types of angiograms may be studies of blood vessels in the brain, eye, lung, kidneys, or other parts of the body. However, this discussion is focused on coronary angiogram, the blood vessel around the heart. A coronary angiogram is usually carried out in a cardiac catheterization lab. This is usually carried out at the same time as angiography.
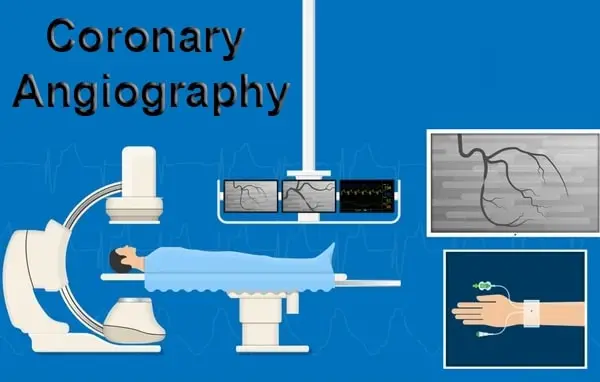
What happens during coronary angiography?
The doctor will make a small puncture in your skin and insert a catheter (a long, thin, plastic tube) into a blood vessel. The doctor will carefully guide the catheter up into your heart. You may feel some pressure in your groin area when the doctor is advancing the catheter. This is normal. Let your doctor know if you feel any pain in your chest, arm, jaw, or throat. These sensations may be a sign that the catheter is touching a blood vessel. Upon arrival in the catheterization lab, you will change into a hospital gown and remove any jewelry. You will be asked to lie on a procedure table. A nurse will connect you to several monitors, which will be used to check your vital signs (heartbeat, blood pressure) during the procedure. Local anesthesia will be used to numb the area in your groin where the doctor will be working. You will be awake during the procedure. However, the amount of sedative given will vary, depending on whether you are having an angiogram because of a recent heart attack or unstable angina. During coronary angiography, you’ll be closely monitored and cared for. This test is usually done in a catheterization lab in a hospital. You will be asked not to eat or drink anything for 6 to 8 hours before the procedure. In most cases, you will need to stay in the hospital overnight. But if your angiography is scheduled late in the day, your doctor may ask you to stay overnight before the procedure.
How long will an angiography take?
After the procedure, patients are moved to a recovery room and are observed. They can often remove the sheath in common femoral artery themselves at the end of the observation period, and then the puncture site is uncovered for another 2-5 hours. Observation time is highly variable depending on the nature of the angiography and the clinical condition of the patient. Ambulatory patients without adverse symptoms may leave the hospital after an hour of observation. Inpatients may return to their hospital room after 4-6 hours of observation. If the patient was admitted purely for the angiography and it was uncomplicated, they are generally discharged later that day. As with any procedure, there are risks of both inpatient and outpatient angiography, that could lead to a significant change in the duration of hospital stay. If a significant procedure such as angioplasty, stenting, or thrombolysis is performed as a result of the angiography, the length of stay can be 1-2 days longer than procedural counterparts.
When can I go home after angiography?
Depending on the type of procedure done, some people can go home the same day as their angiogram, while others may need to stay in the hospital overnight. Those who have an angioplasty and stent usually need to stay in the hospital for 1 to 2 days. Although this is done through a puncture in an artery in the arm or leg, it is still important to remain still for several hours after the procedure to decrease the risk of bleeding at the catheter site. Activities after going home can usually be done as the person is able to do. Restrictions are typically related to not lifting heavy objects or things greater than 10-15 pounds and not lifting the arm above the shoulder if the puncture was in the arm. Medication is not usually prescribed after the procedure to have an effect on the ability to care for oneself. Most people who have angiography have a rapid recovery and are able to return to their usual activities within a few days. Follow-up care after angiography and potential interventions is based on the clinical findings that were unveiled. This would be a topic to discuss at the time of the procedure or at the time of the follow-up visit.
Risks involved with angiography and angioplasty
Iodine contrast medium can cause an allergic reaction in approximately 1 in 40 patients. While most of these reactions are mild, it is important to be vigilant as severe reactions can occur and very rarely, death. Allergy to contrast medium is not an issue with angiography alone. Venous thrombosis, contrast medium inadvertently injected outside the coronary arteries, and radiation exposure to the testes with potential effects upon future fertility are other rare complications of angiography. High quality referrals to the cardiologist can minimize the chance of these adverse events by ensuring that the test is performed in an appropriate patient and that the most experienced operator available carries it out. Simulation with a non-invasive test before angiography is another way to reduce the risk of complications, though this must be balanced against the small risk of the non-invasive test itself. Angiography and angioplasty are known as relatively safe procedures. Major complications combine a death rate of about 1 in 500. Stroke is caused in about 1 in 100 people. Heart attack is very rare, while developing a need for emergency bypass surgery is about 1 in 300. Contrast-induced nephropathy is an important cause of morbidity and mortality after coronary angiography. Premenopausal women, patients with pre-existing renal impairment, and people with diabetes are particularly at risk. Measures to reduce the risk of contrast-induced nephropathy include staying well-hydrated and limiting the amount of contrast used.