The Different Types of Hysterectomy and Their Benefits
The Different Types of Hysterectomy and Their Benefits
What Is a Hysterectomy?
A hysterectomy is a surgical procedure in which a woman’s uterus is removed. The uterus is a small, muscular organ in the female pelvis that functions to nourish and house a fetus while it is growing in the mother’s body. Hysterectomies are performed for a wide variety of reasons, and a surgeon may elect to perform a hysterectomy as an emergency, life-saving procedure. Alternatively, a hysterectomy may be an elective procedure in which the woman and her healthcare provider decide that this surgical intervention is the best option for her long-term health. Hysterectomy is the second most commonly performed surgical procedure (after cesarean section) for women of childbearing age in the United States, where about 1 in 3 women undergo a hysterectomy by the age of 60.
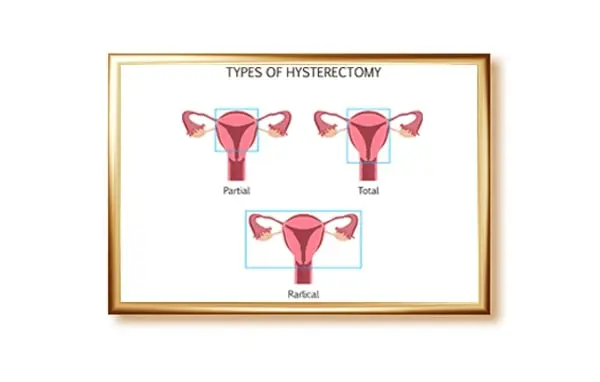
Types of Hysterectomy
Your surgeon might recommend this type of hysterectomy based on your personal health history. For instance, if you’ve had extensive scarring from prior surgeries, such as surgery for fibroid removal. This approach involves removing the uterus and cervix through the vagina. If possible, in some cases, the uterus is cut into smaller pieces before it’s removed. This type of surgery is often performed for noncancerous conditions as it is used to remove the uterus through the vagina. This alone, however, should not be interpreted as cancer not being present. A radical hysterectomy removes the uterus, cervix, upper part of the vagina, and surrounding tissues. Be sure to talk to your doctor about what will be done with your fallopian tubes and ovaries. These structures are often removed at the time of this surgery. This type of hysterectomy is usually recommended when cancer is present. Typically, this type of surgery is performed with a larger abdominal incision, and it requires a longer recovery.
Hysterectomy is a treatment for a variety of conditions, including certain types of cancer, long-term pelvic pain, and abnormal bleeding. Some conditions that require hysterectomy can be life-threatening. There are different types of hysterectomy. All types are available using minimally invasive surgical techniques, such as with a laparoscope or robot. Some types of hysterectomy may be done through the vagina. Others are done through a larger abdominal incision. Less invasive types of hysterectomy may have benefits, such as shorter recoveries. But more complex conditions are more likely to require more extensive hysterectomies. Talk to your physician about the best type of hysterectomy for you and what to expect. A total hysterectomy removes the uterus and the cervix. A partial hysterectomy removes only the uterus and leaves the cervix in place.
Surgical Techniques for Hysterectomy
Traditional approaches to hysterectomy – vaginal and abdominal – may be combined with laparoscopy. Of the 600,000 hysterectomies performed in the United States each year, about 70 percent are abdominal and 25 percent are vaginal, with the remaining 5 percent done laparoscopically. None of the types of surgery is appropriate for everyone. The first choice is always to do surgery vaginally, because it doesn’t require an incision, a patient goes home faster, and she recovers faster. But if the indication is more complex – say a large uterus – usually an abdominal approach is required.
Surgical techniques for hysterectomy broadly include a vaginal approach, in which the uterus is removed through the vagina; an abdominal approach, in which the uterus is removed through an abdominal incision; and a laparoscopically assisted vaginal approach. Each type of surgery has its benefits, and the right choice for you may depend on several factors, including why the surgery is being performed and your individual medical condition. Your doctor will also consider whether the surgery is likely to be straightforward or more complicated, and your own preferences, such as whether you hope for a quicker recovery or place value on feeling little or no pain during and after surgery.
Open Surgery Hysterectomy
The abdominal hysterectomy is usually performed due to high levels of the uterus or large uterus, often because of cancer of the uterus, or often due to adhesions or scarring from past operations that distort the pelvic region. Also abdominal hysterectomy alone is the preferable process for certain women whose abdomen or pelvis has continuous condition through which the operations with minimally do not go. The abdominal alternative additionally is suitable for some overweight with excess quantities of belly fat with uteruses (tummy fat). It is a less popular way at present time, the majority of the hysterectomies in United States arranging with the laparoscopy, and da Vinci process (the procedure carried out by the robot). But, the process certainly leaves a tough surgical scar, hospitalization time significantly increasing it, as well as necessary restoration time.
An open surgery hysterectomy usually is performed if an abdominal hysterectomy is required. The procedure involves making a 5 to 7 inch incision into the bottom of the belly and removing the uterus through it. The major gain of the open surgery hysterectomy is that a surgeon has plenty of space to see and work with the patient’s uterus, fallopian tubes, and ovaries. She/he can control bleeding, protect the bladder, examine other pelvic organs, grooves, and tissue to detect the health issue. The operation may include separating and reconnecting fallopian tubes, if the doctor must remove uterine tubes and cervix. The process takes 1 to 2 hours, and mostly anesthesia is required.
MIP Hysterectomy
Laparoscopic, or minimally invasive (MIP) hysterectomy can often be used instead of traditional hysterectomy. MIP hysterectomy is affiliated with smaller incisions and reduced pain, as well as a more rapid recovery. Unfortunately, not all patients are appropriate candidates for MIP hysterectomy. For example, a patient with a large fibroid uterus may not be a good candidate for MIP hysterectomy because the fibroid uterus may not be able to be removed through the small laparoscopic incision in the abdomen. Most MIP hysterectomies are done with the assistance of a device called a power morcellator. This is a device that cuts large organs into smaller pieces, which can be easily removed from the body through small incisions. Unfortunately, power morcellators can spread the cancerous tumor a patient may have to other parts of the patient’s body. If this occurs, it may make it very difficult, if not impossible, to cure the cancer.
Comparison of MIP Hysterectomy and Abdominal Hysterectomy
The length of the MIP hysterectomy surgical time is approximately 2.5 hours; Although no long-term difference has been noticed between a MIP and abdominal hysterectomy, a short-term one has been demonstrated. The vaginal surgery has a quicker decrease in hemoglobin, requires fewer pain medications, and causes the patient to spend less time in the hospital. The MIP procedure is being utilized to a greater extent than any of the other healthier operations. Even maternal-fetal medicine specialists and gynecologic oncologists, who do not perform this kind of surgery on a regular basis, are finding that it is becoming a more common procedure than an abdominal hysterectomy.
People who follow the evolution of surgery may be aware of many medical advances. In the not-too-distant past, when a woman needed a hysterectomy, it meant a large incision in the abdomen. This resulted in a two-month recovery. With the advent of laparoscopic surgery, the recovery was shortened to six weeks. During the past few years, the technique for using laparoscopic instruments has become so advanced that a new surgery, MIP – minimally invasive hysterectomy, includes the removal of the cervix and uterus through the vagina.
Risks of Hysterectomy
It is unethical to remove healthy organs from patients. Published studies have revealed that 76% of all major complications (e.g., injury to the bowel, bladder, urethra, or major blood vessels) and 90% of minor complications (less serious) occurred in surgeries in which hysterectomy was performed. Hysterectomies were recommended by male doctors who believed the uterus was the most dangerous organ in the female body, and only castration would cure women from mental illness and other non-related to reproductive organs.
Why should we focus on discussing the risks of a hysterectomy? Hysterectomy is the most frequently performed gynecologic surgical procedure, with approximately half a million women undergoing the procedure every year. It becomes counterproductive to inform the public about the lack of long-term consequences of the procedure when the scientific literature and women’s personal experience indicate the opposite. The general topic is about negative results of the procedure on women’s health. Specific problems include bladder, bowel, vascular, and lymphatic system damage, osteoporosis, absent menstruation, menopause, etc. Hysterectomy is associated with many serious adverse effects, both in the short and long term. These risks, both known and unknown, should be thoroughly considered and weighed against the risks of other treatment options, on a case-by-case basis, before a decision is made to remove a normal, non-cancerous uterus.
What to Expect After a Hysterectomy?
Your short-term hysterectomy recovery will likely last about six weeks. This doesn’t mean that emotionally and mentally, you’ll feel back to your normal self, but your body repairs much of the trauma done to it during surgery; at least, as best as it can in a month and a half. There are a few milestones to keep in mind as you heal. After about three weeks, more rigorous activities like picking children up, doing laundry and light housework should be doable without much discomfort or risk of prolonging your hysterectomy recovery. After four or five weeks, intercourse can be resumed, as well as activities like driving and exercising. After six weeks, you can generally ease back into heavy lifting, standing for lengthy periods of time, working and a majority of your other pre-hysterectomy activities.
If your ovaries were removed, you will have immediate symptoms, which may feel severe because they come on so quickly. You may even need pills or patches to replace the hormones your ovaries would otherwise be producing. Because of the lack of hormone, you’ll be at risk for a condition called osteoporosis, which weakens the bones and may affect your ability to walk without pain or risk injuring the bones in a fall; and for fractured bones, which can happen as a result of osteoporosis or from a fall.
The type of hysterectomy you have will determine how long you stay in the hospital and how long it will be before you recover. After a hysterectomy, you’re likely to start menopause if you haven’t already. Whether your ovaries were removed or not, you may have hot flashes, vaginal dryness, mood changes, night sweats, and sleep problems related to this change in life. If your ovaries were not removed during surgery, you may delay menopause by about 2 years. Some types of surgery will also allow for a bit of time before you start these symptoms because they allow the ovaries to stay healthy and continue to produce hormones.